Facing Fear as an Emergency Department Physician During the Pandemic
Rutgers Robert Wood Johnson Medical School professor Kusum Punjabi shares her experience
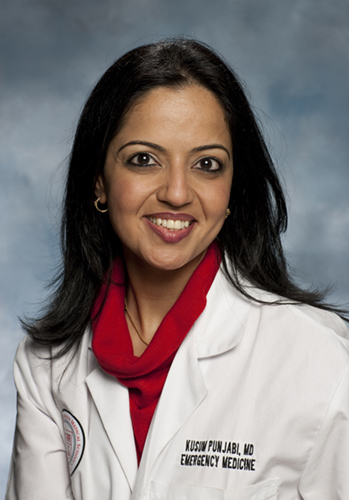
Mask, eye shield, cap, gown, gloves. Evaluate patient. Remove gear. Dispose. Wash hands. Sanitize. Repeat. This has been my norm for the past two weeks for at least 20-30 patients a shift at the Emergency Department (ED) at Robert Wood Johnson University Hospital in New Brunswick, NJ.
I have been an emergency physician for over 10 years. I have been trained to face HIV, Ebola, avian flu, SARS, swine flu etc. But nothing compares to this. In all those situations, the risk of exposure was low as very few patients came to the ED with the symptoms. We were trained in personal protective equipment (PPE) and all appropriate clinical protocols and work went on as usual. This time nothing is the usual.
Two weeks ago when the positive cases first started coming to our ED, we were all working our usual 8-12 hour shifts and seeing 5-10 patients a shift with chief complaints of cough/fever. Most patients were healthy, young, not tested for COVID and sent home.
Now almost every patient we evaluate has respiratory complaints and most of the ones we test are COVID positive.
According to estimates from the Centers for Disease Control and Prevention reported by The New York Times, between 160 million and 214 million people in the United States could become infected with COVID-19 and as many as 200,000 to 1.7 million people could die. Estimates for hospitalizations range from 2.4 million to 21 million people.
Given that in the United States we have only about 925,000 hospital beds and less than 100,000 ICU beds and patients with severe coronavirus often develop pneumonia and require 7-10 days of hospitalization, it’s painfully obvious that hospitals do not have the capacity.
At RWJUH, the hospital administration, particularly our Chairman, Robert Eisenstein, and our CEO, Mr. John Gantner, are constantly working hard in making a variety of preparations for the influx of patients with coronavirus.

In the past two weeks we have created triage tents outside the ED entrances to evaluate patients who are “sick” vs. “not so sick” with respiratory complaints. Patients who are young, healthy and breathing well (>95% oxygenation) are seen via telemedicine (a video connection via a computer or phone – to protect both patients and health care providers) by an emergency physician and discharged from the outside tent with self-quarantine instructions. Patients who are elderly or with abnormal vital signs are brought back into the ED and immediately placed in isolation so as to not contaminate the waiting room. Once in the main ED under full PPE precautions the patient is evaluated and treated.
Sick patients who are admitted for possible coronavirus are tested and treated as per RWJUH infection prevention protocols. At RWJUH, there are special floors dedicated to caring for these patients and special teams of doctors and nurse practitioners trained in wearing PPE responsible for their care.
Patients getting treated for strokes, heart attacks and other non-COVID complaints are placed on other dedicated floors within the hospital to limit contamination with a separate team of doctors and medical staff to care for them. Daily updates and WebEx meetings with hospital administrators/staff help us all stay informed. Through clarity on protocols, we are changing practices daily to adhere to best practices for our patients and ourselves.
As an ER physician, I am nervous, but feel prepared. Two weeks ago I was able to wear a new mask for each patient I was evaluating. Now I wear one single mask for my whole shift to conserve our supplies for the surge in patients that we expect in the coming weeks. While at work I try hard to not touch my face, keep distance from others and practice the utmost sanitation at all times. At the end of a shift, I change out of my scrubs before I come home. Once home, I go straight to take a hot shower before interacting with family and place my scrubs for washing. I check my temperature everyday twice a day to insure I am not getting symptomatic. I do not want to put others at risk.
I am grateful for my job and I feel blessed to be caring for others at this difficult time.