A New Way to Fight Deadly Fungal Infections
Rutgers researchers are developing a broad-spectrum vaccine that could save hundreds of thousands of lives
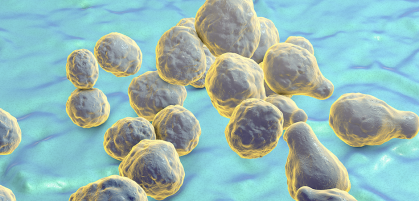
Only a small fraction of the more than one million species of fungi can cause infectious disease in humans. But for the growing population of people with weakened immune systems in the United States and around the world, a fungal infection can be serious, even deadly, as evidenced by recent outbreaks in health care facilities.
Many serious diseases, such as smallpox and polio, have been totally or mostly eradicated through vaccines. However, vaccinating against fungal infections is not a treatment option. Rutgers researchers are working to make it one.

Chaoyang Xue, a microbiologist and associate professor at Rutgers’ Public Health Research Institute, runs a lab dedicated to understanding the pathogen Cryptococcus neoformans, the leading cause of the fungal brain infection cryptococcal meningitis, which annually kills more than 180,000 people worldwide, according to the Centers for Disease Control and Prevention.
Xue and Amariliz Rivera, a fungal immunologist and assistant professor at New Jersey Medical School, are developing a vaccine to prevent these deadly fungal infections. A big-impact project in its early stages, the research drew the attention of Rutgers’ TechAdvance program, which helps move promising technology in the direction of commercialization.
Xue and Rivera (pictured above: right and left) took a break from laboratory work to speak with Rutgers about creating solutions that go beyond treating fungal infections—to preventing them through vaccines.
Rutgers University: Why are fungal infections so difficult to treat?
Chaoyang Xue: Fungi, generally, have a complex cellular organization, just like humans. We actually share a lot of the same cellular mechanisms with fungi. So, when treating a fungal infection, if you target something that kills the fungus, it may have a greater side effect on the human host because of shared cellular mechanisms.
RU: What fungal infection treatments are available to patients today?
CX: No vaccine is available for clinical use, so right now patients are limited to mainly three classes of antifungal drugs. All three of these classes are useful, but they each have their limitations.
RU: Why is an antifungal vaccine needed?
Amariliz Rivera: There is a big gap between what is needed and what is available. Right now, antifungals are mainly delivered by intravenous infusion. This is an obstacle in many regions of the world where invasive fungal infections are prevalent, but public health resources are limited. Due to these limitations, the mortality rate for invasive fungal infections, such as cryptococcal meningitis, remains unacceptably high.
CX: Also, antifungal drugs must be used over a long course of time, which is costly—in terms of resources and money—and because extended exposure may lead to increased drug resistance. A simple vaccine would potentially overcome many of these issues, which is why we think it should be a valuable alternative for treating fungal infections.
RU: Viral and bacterial infections are well understood to be a tremendous global burden. Fungal infections are also a significant burden on human health but are far less recognized. Why?
AR: In part because of a lack of awareness on the detrimental impact of fungal pathogens to human health. The rise of fungal infections is a relatively recent phenomenon, when compared to something with a well-known historical impact, like tuberculosis or flu. As medical interventions have improved and new medications are developed, immune-suppressive regimens can increase susceptibility to fungal pathogens. Therefore, the incidence of these infections has significantly increased and is expected to continue to grow.
RU: How close are we to having a vaccine available?
CX: We have identified and submitted a patent on a heat-killed fungus strain that is a good vaccine candidate. Our preliminary findings suggest that this vaccine strain can protect against multiple types of fungal infections. This is potentially very useful if we could develop a single vaccine to treat multiple systemic fungal infections. Given current data, our plans are to improve the vaccine formula and delivery method, and conduct preclinical toxicity studies before moving to the next step, which is a clinical trial. We are actively looking for potential industry partners to further develop this vaccine.
RU: What is it like being a researcher at Rutgers?
CX: The great part about Rutgers is that there are a lot of resources available and a really strong research environment. I have many colleagues who share common research interests in infectious diseases. I really enjoy what I do.
AR: I did my doctoral studies at Robert Wood Johnson Medical School and have thus been very familiar with the excellence in research at Rutgers for a long time. Coming back home to Rutgers as a faculty member at New Jersey Medical School was a dream come true.
>> Learn more about Rutgers' Public Health Research Institute
First published on October 7, 2019. Interview by James Foley, Rutgers University Communications and Marketing. Title image via Shutterstock. Portrait images supplied by Amariliz Rivera and Chaoyang Xue and used with permission.