Rutgers Neurologist Explores Link Between COVID and Brain Fog, Dementia
A new Rutgers study led by a leading neurologist who is an expert on aging will examine the effect of COVID-19 on memory loss, dementia and brain fog.
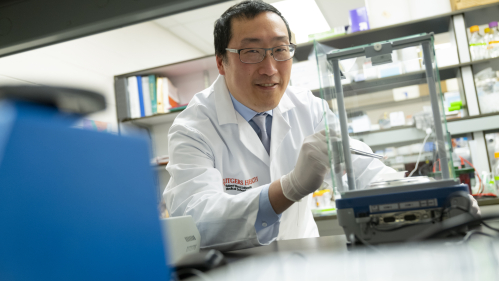
“Many people who recover from mild or moderate COVID-19 notice slowed thinking or memory loss, and this motivated us to leverage our experience in studying cognitive issues related to Alzheimer’s disease, multiple sclerosis, and HIV to examine this phenomenon,” said William T. Hu, associate professor and chief of cognitive neurology at Rutgers Robert Wood Johnson Medical School and the Institute for Health, Health Care Policy, and Aging Research. Hu is a leading cognitive neurologist and neuroscientist who has been studying cognitive impairments following mild to moderate COVID-19 at Rutgers.
“We have found neuroinflammation is a common theme across many brain disorders, but not all neuroinflammation is the same,” he said. “We developed a roadmap to study the protein and cellular changes involved in worsening – as well as alleviating – symptoms of brain fog. In addition, we are using the latest RNA sequencing technology to understand how inflammatory cells ‘misbehave’ to cause memory/thinking dysfunction in long COVID.”
Hu’s team will assess each person’s cognition, mood, and sleep patterns to identify potential causes of brain fog and compare their brain MRI findings with biochemical signatures of neuroinflammation. They will analyze microglial cells – critically important immune cells in the brain – from individuals who have had COVID-19 to determine whether those cells can be used to predict the persistence of post-COVID cognitive impairment (PCCI). This will allow researchers to determine why these cells may dysfunction in COVID-19 and PCCI, what the shared inflammatory mechanisms are between PCCI and Alzheimer’s disease, and whether FDA-approved drugs can be repurposed to prevent the onset of PCCI or improve its outcomes, Dr. Hu explained.
Hu recently received $100,000 in grant funding from TMCity, a private foundation based in Irvine, Calif., to help support the project, which also will address whether COVID-19 infection accelerates the clinical manifestation of Alzheimer’s disease in people age 50 and above who otherwise would not have demonstrated symptoms until their 60s and 70s.
“Generous support from TMCity will accelerate this effort in New Brunswick with the potential of applying the technique more broadly to other organs affected by long COVID, such as heart and lungs,” Hu said.
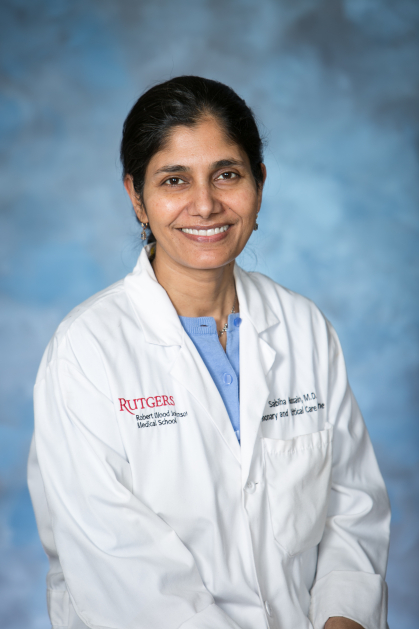
The study builds on work Hu and his team have been doing with the growing Post-COVID Recovery Program led by Sabiha Hussain, associate professor of medicine in the Division of Pulmonary and Critical Care at Rutgers Robert Wood Johnson Medical School.
The program, which is a joint initiative of the medical school and Robert Wood Johnson University Hospital, typically sees 15-17 people in its weekly Monday clinics and provides a range of services, including behavioral health; cardiology; cardiac and pulmonary rehabilitation; physical, speech and occupational rehabilitation; nutritional services; pulmonary/sleep therapy; and assistance with financial and social barriers related to recovery, in addition to the cognitive assessment and therapy that Hu and his team provide, with additional assistance in cognitive rehabilitation from the Kessler Institute for Rehabilitation.
Approximately half of the individuals who have been seen in the program have issues with brain fog after their bout with COVID. Of those who screened positive for neurocognitive issues, symptoms include memory loss, brain fog, new confusion, headaches, numbness, and multiple neurological symptoms, Hussain said.
“Neurocognitive consequences of post-COVID syndrome affect the daily life of 62% of our patients,” she said.
“The vaccine may have helped somewhat with the brain fog, but what I see from a clinical standpoint is much more persistent short-term memory loss,” said Hussain, who also serves as the medical school’s director of interventional bronchology, as well as its Adult Cystic Fibrosis Program.
She stressed that the clinic is open for anyone who had COVID, regardless of whether they’re having active symptoms. “What we’re finding is that they may not have respiratory symptoms or issues that would alert them to say, ‘Hey, I need to go see a physician,’ but they have other underlying symptoms like a lot of fatigue, neurocognitive issues, and depression and anxiety that they don’t understand exactly why it is happening. We screen for all of those things, which helps with overall quality of life,” Hussain said.