Is Menopause Having Its Moment?
If you are a woman between the ages of 40 and 60, there’s a topic that is likely taking over your group chats, social media feed and dinner party conversations: menopause.
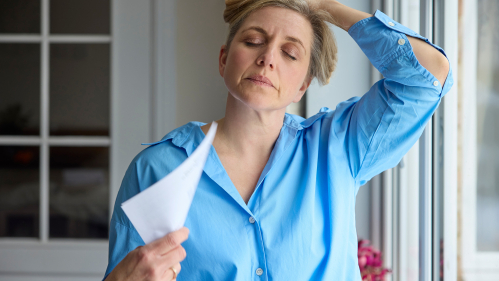
It’s a subject previously discussed in hushed tones – if at all. But these days, everyday folks, influencers and medical experts alike are talking about the many frustrating symptoms associated with perimenopause and menopause – hot flashes, mood swings, anxiety, joint aches and pains, insomnia, decreased libido and weight gain, to name a few – and how to treat it.
From Instagram influencer Melani Sanders’s viral “We Do Not Care Club” to menopause expert Mary Claire Haver’s book, The New Menopause, and multiple celebrities and content producers in between, throngs of women are addressing “the change” out in open, using humor, research and camaraderie to cope with and find relief from their symptoms.
We spoke with Gloria Bachmann, professor, co-director of the Women's Health Institute, and associate dean for Women's Health with Rutgers Robert Wood Johnson Medical School whose career as a ob-gyn spans four decades, about why conversations about menopause are becoming mainstream, and why women shouldn’t suffer in silence.
Is menopause having a moment?
I don’t know if it’s menopause, specifically. It’s more particular to all of us now accepting aging in all persons, and not associating menopause with a woman being ‘old.’ If we go back over history, menopause meant you’re old. That was the definition before. If someone were 45 and not having periods, they wouldn’t talk about it because they didn’t want people to know, “I’m over the hill,” as they used to say, or not as much of a woman as I previously was. I think we’ve gotten away from that. Now women are more open to talking about menopause. It doesn’t mean you’re washed up. It’s just another part of our life cycle.
What do you think caused the shift?
I think it’s two-fold. First, society does not look at menopause in such a negative way anymore. We now have many role models who are in their 50s and 60s, and they’re not considered old. They are still seen as attractive and productive. Many actors and political individuals are of menopausal age, and we still respect them very much. Secondly, science has continued to study menopause, and this new research has refuted the early negative data on menopausal hormonal therapy.
Are more women treating their perimenopausal and menopausal symptoms with hormone replacement therapy (HRT) now than in the past? If so, why?
In the distant past, hormone therapy was given out to almost all women experiencing perimenopause and menopause symptoms: hot flashes, mood swings, problems sleeping, anxiety, and just feeling lousy. That was before the Women’s Health Initiative (a series of clinical studies started in 1991 to understand health issues causing morbidity and mortality in postmenopausal women) put a damper on this management. However, that research data was not fully evaluated and it basically frightened society – not only women, men, too – by saying if you take hormone therapy, you were at an increased risk of developing cancer. But the bottom line is there were many, many other factors to consider. The data really should have been evaluated more thoroughly before blanket statements were put out.
When did physicians begin using HRT again to treat these symptoms?
It’s been gradual. We’ve had more data on its benefits overall and we’ve also reevaluated the Women’s Health Initiative. As well, I believe women’s health is being taken more seriously now. Menopause and the changes women experience are now evaluated fully rather than dismissed. And every woman has a different experience, but many have very negative experiences and hormone therapy can help manage these symptoms.
What are the benefits of hormone therapy?
The major benefit is addressing the symptoms. I don’t want to minimize that so many women are being told, ‘You can grin and bear it. Why do you need it? Just put a lot of fans in your house, throw the covers off when you’re sleeping.’ That is something that has to be stopped. Hormonal therapy is important for controlling debilitating symptoms for so many menopausal women.
I think the bottom line here for women is don’t hesitate and say, "'Let me see if it will go away."’ Start earlier and don’t wait until you are miserable because the data all point to the fact that you want to start within 10 years of your menopause and before 60 years old to minimize your risks. It does relieve many of the perimenopausal and menopausal symptoms, plus it protects against osteoporosis and reduces risk of cardiovascular disease.
What are the risks?
What I tell every individual is that for anything we do there is a risk vs. a benefit. When you get into your car, you can have a fatal accident. But the risk is small if you follow all safety precautions and don’t drive dangerously. Doctors look at the individual and make sure the benefits outweigh the risks for any intervention. And the benefits of hormone therapy for perimenopausal and menopausal women under 60 years of age definitely outweigh the risks for almost all women.
Which women are the exception?
I tell everyone if you have family history of breast cancer you should have genetic testing, as you are already at risk for breast cancer. After age 60, you could already have cardiovascular disease or be at risk for stroke if you have a history of blood clots. But if you are under 60, your mammograms are up to date, you have not had cancer and you are in good health, the risks are minimal, but the benefits are great.
What if you are not at risk and your ob-gyn will not prescribe HRT? What are your thoughts on turning to all-virtual menopause health care?
I think every practice that deals with women – ob-gyn or general practitioner – does prescribe for menopausal symptoms. All the clinical teams at Rutgers do. But it’s like anything else in life, if your store doesn’t have what you need, go to another store. Don’t stay with a clinician who does not respond to your needs. However, it’s best to stay with the clinician who is doing your pap test and writing your mammogram scripts. You don’t want to separate overall gynecological health from menopausal health.